T: 01822 851370 E: [email protected]
Visit RSN Survey about life in rural England to find out more.
March Edition of Casebook from the Rural Health and Care Alliance
March 2022 Edition
In Casebook this month, some interesting stories about a resilient coronavirus, the impact of rising prices and a shortage of dedicated facilities on mental health in rural setting and an emerging agenda for our work next year.
NEWS COMMENTARY
Would-be paramedics hit with £27,500 bill to retrain for vital service
I suspect this unfortunate situation will impact the pipeline of parademics available in rural settings. This story tells:
Professionals who want to retrain as paramedics are facing tough financial decisions after discovering they are barred from government funding.
Many who were inspired by the pandemic to join the NHS say they are being treated as second-class applicants because an outdated policy has excluded them from loans and grants available to almost all other mature healthcare students.
Since September, trainees must complete a university (BSc) degree to qualify as a paramedic. However, paramedic science, unlike other NHS professions, is ineligible for a student loan if studied as a pre-registration (second) degree course in England. Those wanting to join ambulance crews face £27,500 tuition fees.
They are also barred from receiving a £5,000-a-year NHS maintenance bursary launched in 2020 to encourage healthcare recruitment. Most pre-registered students studying related subjects are eligible for the money, which is not means tested. Mature students in Scotland, Wales and Northern Ireland qualify for varying degrees of government support.
The English funding anomaly means that a paramedic seeking to retrain as a nurse or a dentist can apply for a student loan and an NHS learning support grant, whereas a nurse or dentist who wants to retrain as a paramedic will have to fund fees and training expenses, as well as living costs, themselves.
Full article: https://www.theguardian.com/money/2022/mar/13/would-be-paramedics-hit-with-27500-bill-to-retrain-for-vital-service
‘Pandemic is not over’: ministers criticised for scrapping UK Covid surveillance
Have we taken our foot off the gas too soon??
Ministers have been accused of “turning off the headlights at the first sign of dawn” after scrapping nationwide Covid surveillance programmes, with scientists saying it will almost certainly end up costing more money in the long run.
Last week, scientists announced that the React study – which randomly tests about 150,000 people across England each month to see how many are infected with coronavirus – will be scrapped at the end of March, and no further data will be collected beyond that point.
Funding is also being withdrawn from the Zoe covid symptom study, the Siren and Vivaldi studies (which monitor infections in health workers and care homes) and the CoMix social contacts survey, while mass free testing is due to end on 1 April.
The Office for National Statistics’ Covid infection survey, which regularly samples the same 180,000 people to estimate what percentage of the UK populations is infected, will continue.
It comes as growing numbers of new infections in multiple countries led one expert to prompt speculation that Europe could be at the start of a sixth wave of Covid infections, partly driven by the “stealth” BA.2 Omicron variant.
Full article: https://www.theguardian.com/world/2022/mar/13/pandemic-is-not-over-ministers-criticised-after-scrapping-uk-covid-surveillance
What is Deltacron? Everything you need to know about the new Covid-19 variant
This virus just refuses to be shaken off and with mutations like this I worry that another bleak winter for rural dwellers could be in store. This story tells us:
A fresh reminder that the pandemic is not yet over comes as new Covid-19 variant Deltacron is officially identified with cases confirmed in France and the US.
Deltacron is a Covid variant that is made up of elements from both Delta and Omicron. It contains genes from both of these previous variants, which makes it a recombinant virus.
This is when the genetic material from more than one origin is combined- in other words, when someone is infected with two variants at the same time and their cells then replicate together.
Full article: https://www.independent.co.uk/news/health/deltacron-covid-variant-pandemic-b2034386.html
‘Inadequate’ children’s mental health hospital ‘put safety of patients at risk’ CQC report finds
Services for children with mental health challenges are rarely discussed. For rural dwellers they are few and far between and we often end up with major dislocation for people wanting to access services and their families. This story reminds us that where these services do exist they are sometimes contested in terms of their effectiveness. It tells us:
Serious safety concerns have been raised about a children’s mental health hospital where staff lacked respect for patients, as the provider faces a police investigation into another one of its units.
The concerns about this hospital come as The Independent revealed police have launched an investigation into another mental health unit run by the provider.
Full article: https://www.independent.co.uk/news/health/huntercombe-hospital-stafford-cqc-b2032429.html
Tenants face having to find extra £1,000 for 2022 rent and bills
This story, filtered through the lens that it is more expensive to live in rural setting in terms of both rent and utilities is worrying. There is strong evidence that the quality of housing impacts on the mental health and well-being of residents.
It tells us:
Tenants already struggling with the cost of living crisis typically face having to find an extra £1,000 this year to cover higher rent and essential bills, research shows.
The estate agent Hamptons said tenants’ finances faced a record squeeze as higher rents and energy bill increases combined to pile more pressure on households in Great Britain.
Recent research from other property firms such as Rightmove has already shown that rents have been rising at their fastest rate on record as tenants making plans for a post-pandemic life jostle for properties. In its latest monthly lettings index, Hamptons said this strong growth led to the average household in Great Britain spending 42% of their post-tax income on rent in 2021 – the highest proportion since its records began in 2010.
When other costs such as gas, electricity, council tax, broadband and a TV licence were included, it meant a typical household spent 52% of their post-tax income on rent and bills in 2021.
Full article: https://www.theguardian.com/business/2022/mar/14/tenants-face-having-to-find-extra-1000-for-2022-rent-and-bills
MEMBER ARTICLES
We’d love to hear from you - share what you’re proud of
If you have something you would like us to feature in a future edition, please let us know by clicking here to send us an email.
This month we have two member articles from the University of Central Lancashire and YMCA Lincs, plus an exciting rural world health event in Ireland.
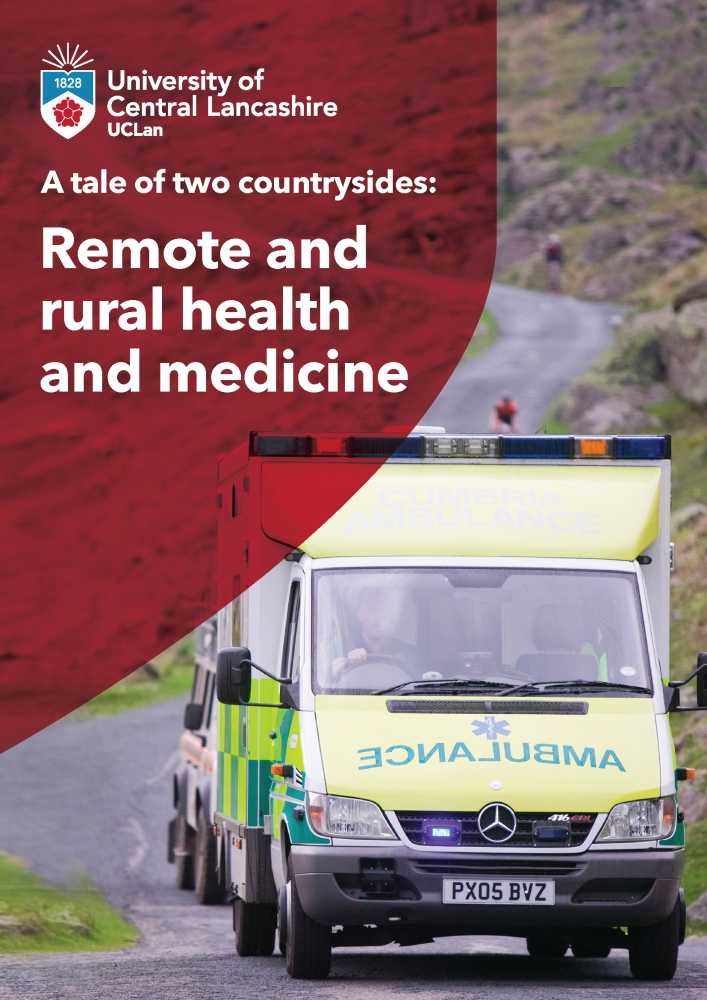
- UCLan researchers reveal stark inequalities between rural and urban communities in the UK, particularly in the North of England
- The new report finds that rural areas are impacted by ‘diseases of despair’, slow advances in health technology, and a lack of healthcare professionals
- Researchers call for more investment into rural healthcare and education to improve health equality
A report commissioned by the University of Central Lancashire’s (UCLan) National Centre for Remote and Rural Medicine has revealed the health inequalities experienced by people in the UK’s rural areas.
The research, published in a report today, analyses the unique health problems prominent in remote parts of the UK. It spans the country, pulling results from all corners of the UK including Jaywick in Essex, Blackpool in Lancashire and up to Copeland in Cumbria, and outlines the measures that are needed to tackle the problem head-on.
In collaboration with local government, educators, industry and politicians, the paper makes the case for a focus on improving health in remote and rural areas. By contrasting coastal towns with market towns and their hinterlands, the paper gives a measure of how far we have to go to “level up” local communities.
For the research, the team analysed a number of available indicators including life expectancy, cancer survival, admissions and readmissions to understand more about health inequalities and the healthcare system in rural areas.
Researchers found that rural areas are disproportionately affected by ‘diseases of despair’. In County Durham in the North East, the rate for alcohol-related-harm hospital admissions was 758 per 100,000 population – significantly worse than the average of 664 per 100,000 for England. This represents 3,972 admissions to hospital per year. The rate for self-harm hospital admissions is 197 per 100,000 population, representing 1005 admissions per year.
Meanwhile, it also found that rural health technology was developing at a slower pace than that in towns and cities, leaving its inhabitants geographically isolated and lonely. While much has been done to improve UK-wide connectivity, rural communities still face problems. According to the UK’s communications regulator Ofcom, 234,000 people in rural England are unable to receive decent broadband from a fixed line. Meanwhile, large rural areas in the north of England and in the southwest are unable to get outdoor 4G coverage.
Further problems were exposed when the researchers looked at the demographic make-up of rural and coastal populations, which were found to be aging twice as fast as the UK average. The proportion of residents over 65 in Richmondshire District Council in North Yorkshire rose from 15% in 2001 to 21% in 2018, according to research from the Resolution Foundation published in October 2019. The average age in North Norfolk is 53.8 years, the oldest average of any local authority.
The worst health outcomes were found in the UK’s seaside towns in terms of mental health problems, more homeless people and more alcohol and drugs problems.
Dr Vincent Argent, Consultant in Rural Emergency Medicine at Dorset Rural County Hospital, says access to health services intensifies the problem:
“Our health services often have poor access because, of course, they’ve got the sea on one side of them. They don’t have 360-degree catchment and, quite often, the roads to seaside towns are not very good – there aren’t any seaside towns that have a motorway coming into the centre of town. Places like Hastings and Rhyl are quite difficult to get out of. People often don’t have jobs, so they don’t have cars, and the public transport is inadequate.”
Added to this is the challenge of recruitment. Rural hospitals were found to be struggling to find consultants to fill their vacancies across the country, with some hospitals not able to fill a single vacancy in a year. A recruitment crisis amongst senior clinicians was revealed in research by
the Royal College of Physicians published in October 2019, showing that just 13% of consultants appointed in England last year went to hospitals serving mainly rural or coastal areas, with the other 87% being hired by those with mainly urban populations.
Areas most affected by health inequalities
While rural Clinical Commissioning Groups (CCGs) have better or similar outcomes to urban ones, likely due to being generally more affluent, huge health inequalities remained in many areas. A spotlight was shone on Cumbria, a region with striking inequalities and diverse geographies. To the east and south of the county, including the Eden Valley and Appleby-in-Westmorland, communities are generally affluent and life expectancy is long. However, to the west, there are small towns all along the coast with significant deprivation. In the borough of Copeland, for example, the rate of alcohol-related admissions is 774 per 100,000 population – worse than the average for England. The rate of alcohol-related admissions in South Lakeland is better than the average for England – 539 per 100,000 population.
Similar differences can be seen across child health and life expectancy not just between those two boroughs but also between Eden and Barrow-in-Furness. The rate of child obesity among children aged 10-11 in Eden is 16.2% compared to 25.5% in Barrow-in-Furness. Life expectancy in Eden is 82.0 years, while life expectancy in Barrow-in-Furness is only 77.1 years. This highlights the existence of pockets that often get overlooked when it comes to rural medicine, indicating that a more unique approach to rural healthcare is needed.
The report identified five solutions for achieving an equitable health service for everyone:
- Better training for rural clinicians
- More training for pharmacists and professions allied to medicine
- Connectivity in rural areas to reduce isolation and accelerate the uptake of digital health solutions
- Accelerate digital uptake and training on digital health skills for clinical workforce
- Solve the recruitment crisis in rural areas by incentivising clinicians to take rural jobs
Professor Catherine Jackson, Executive Dean, Faculty of Clinical & Biomedical Sciences and Head of the School of Medicine at UCLan, said:
“Because doctors now specialise at a much earlier stage than they used to, both primary- care and secondary-care doctors feel uncomfortable in a remote and rural setting. Primary-care doctors of my generation who went to work in remote and rural locations had usually all done something else beforehand – they’d been a surgeon or an anaesthetist or, as in my case, a physician – so they brought additional experience. Because of the training routes for doctors that increasingly doesn’t happen anymore.
“At UCLan, we’ve created a number of courses specifically designed to train remote and rural practitioners, basically wherever help isn't coming very quickly. They could be working here in the UK or on oil platforms or in the middle of the desert or in an aeroplane. It’s to provide people the skills and competencies and confidence to practice, so they feel able to go and work in these places – to be able to practice safely and to provide a very good standard of care. If we want to successfully level up these regions, we need to be able to offer a first-class service, but it has to be delivered differently in order to address the specific challenges.”
- The full report can be read here
| ? |  |
YMCA Lincolnshire’s TED (Talk, Eat, Drink) in East Lindsey programme is one of 14 Ageing Better programmes across England, funded by the National Lottery Community Fund
It delivers from Louth, Mablethorpe and Skegness to villages and sparsely-populated rural areas
TED has reduced social isolation and loneliness in those aged 50 and over. It commissions delivery partners on specialist projects including Digital Skills, Citizens Advice and activities for male carers. TED also delivers a Befriending Service, Friendship Groups and an Age-friendly Business Award.
With the programme set to end at the end of March, YMCA Lincolnshire’s Communities team held a TED Celebration Event at Embassy Theatre, Skegness on Wednesday 10 March. Volunteers, service users and delivery partners enjoyed an afternoon of reflection and appreciation, as Councillor William Gray praised the success of the programme.
The team has risen to the challenges these rural and coastal communities have presented, supporting the mental and physical wellbeing of older people in East Lindsey. This was key during a pandemic which required a shift to different methods of delivery.
Chief Medical Officer, Prof. Chris Whitty’s 2021 Annual Report, focusing on Health in Coastal Communities, referred to TED’s impact in communities across East Lindsey. It has been a catalyst for change in the district, contributing to the evidence base and best practice when working with ageing communities.
The sparsest coastal areas struggle to access services and public transport links are often poor. This can leave those aged 50 and over even more physically and emotionally isolated. They may feel ‘trapped’ where they live, with limited chances to move away or see other places. The Centre for Towns added in 2020 that “coastal towns are the most isolated of all place types.”
The Report showed how TED had mitigated COVID-19’s impact on coastal communities in East Lindsey, by providing connection and preventing isolation.
Whilst the programme ends in March 2022, YMCA Lincolnshire’s Communities team is well-placed to continue making a positive impact on residents’ lives. The team hopes this recognition will lead to similar partnerships in the future.
Over one-third of East Lindsey’s population is over 60, with 80 per cent living in rural areas. Thus, TED’s work in the district has been appropriate, targeted and needed.
In 2020 an Ageing without Children online support group was established, led by a person with lived experience and facilitated by stakeholders. This recognised recent lockdowns left older people relying on family connections and presented yet another challenge for those living alone.
A collaboration with the Healthy Ageing Research Group at the University of Lincoln has researched the experiences of people ageing without children in East Lindsey. This work showed how social connections can positively affect mental and physical health and raise awareness of health challenges relating to isolation and loneliness.
YMCA Lincolnshire’s Communities team is using lessons learnt from TED to inform future projects that will engage ageing communities across Lincolnshire.
To find out more visit: YMCA Lincolnshire - Welcome to the Lincolnshire YMCA (lincsymca.co.uk)
NATIONAL CENTRE UPDATE
Here are four things we would like to achieve in 2022, all inspired by our Parliamentary Inquiry. If you are interested in joining in please let us know:
1. Piloting of the National Centre for Rural Health and Care Toolkit (Parliamentary Inquiry recommendation 4)
We have 4 early adoption areas on standby to implement the rural health and care toolkit, develop with Rural England. They are: Devon, Lincolnshire, Suffolk and Shropshire. Output 4 detailed case studies and the directly positive health outcomes arising in these settings.
2. Develop a curated network for innovative primary care centres which are community focused (Parliamentary Inquiry recommendation 12)
Identifying and sharing best practice about multi-agency working, self-care and increased health literacy in relation to rural health inequalities. We intend to have an initial focus on coastal settlements associated with the key health workforce challenges identified in the PMOs 2021 report. Output a gazeteer of best practice and a fully functioning and self supporting ongoing network.
3. Create a knowledge exchange of good practice and problem solving focused on the rural challenges associated with the interface between health and care (Parliamentary Inquiry recommendation 10 and 11)
We will undertake detailed research across England and follow the international good practice leads arising from the Parliamentary Inquiry to look at writing up and sharing examples of where dislocation at the interface of health and social care, in the context of local delivery blight desired outcomes. This will focus on more effective resourcing of early discharge from acute settings, the most effective examples of staffing of domiciliary care and the effective use of technology to support innovation. We will not only create a repository of good practice but we will create a self supporting network of rural ICS interested in this theme, beginning with our own membership, but open to all. Outputs detailed report covering best practice and a dedicated ongoing community of practice.
4. Create a rural mental health network (Parliamentary Inquiry cross cutting)
There is significant recognition of the need for a good practice and network facility to address the particular nature of rural mental health. The Scottish national rural mental health strategy has delivered a real impetus in terms of the recognition of this issue and has driven preventive improvements and a recognition of the importance of this issue from a workforce perspective, both in terms of the skills needed to address mental health challenges in rural settings and the mental health challenges facing rural health practitioners. Output, Rural Mental Health Strategy and good practice dissemination materials and plan.
FUNDING OPPORTUNITIES
This month we focus on four funding streams:
- The Prince’s Countryside Fund – Making a long-term difference in rural communities
- The Asda Foundation – Empowering local communities
- The National Lottery Community Fund – Social enterprise support
- Medical Research Council – Applied global health research funding
To find out more about each of these funds click here
Spread the word
If you know of other organisations that you think would benefit from joining the Rural Health & Care Alliance, please click here to email us and let us know.
RURAL SERVICES NETWORK
Up to date news on Health and Care
The Rural Services Network provides a useful source of themed news content and data. Check out the latest news on Health & Wellbeing and Vulnerability, where you’ll find articles on a diverse range of rural issues affecting rural communities. You might also find this research on Over 65 Population Projections useful too.
Latest from RSN Member Insights
RSN Member Insights is the place to discover the statistics that define communities within our membership. It is regularly updated with new analyses, and these will be highlighted in the 'What's New' section of the RSN's Weekly Rural Bulletin. The Rural Bulletin also provides a selection of the most rurally topical news items, so do subscribe and encourage your colleagues to subscribe to what is an invaluable weekly periodical.
To make a suggestion of data that would benefit you by being included in the Member Insights section, please email Dan Worth, our Research and Performance Analyst, at [email protected].
| The Rural Health & Care Alliance is a membership organisation administered by the Rural Services Network on behalf of the National Centre for Rural Health & Care. Explore the RHCA service below: |
 |
 |
 |
 |
 |
 |
 |
 |
 |
 |






