T: 01822 851370 E: [email protected]
Visit RSN Survey about life in rural England to find out more.
Casebook - March 2019
Casebook is a monthly service for members of the Rural Health and Care Alliance. It summarises 5 current news stories, along with other relevant content.
March 2019 Edition
In this edition of case book we look at: pressure on the A&E target, unsustainable care homes, the subversively malign influence of junk food adverts, private ambulances and the opportunity to keep tabs on the performance of your local health service.
News
Pilot scheme moves NHS closer to ending four-hour A&E target
Did you know that hospitals which are more than an hour from the next nearest acute setting are described in NHS jargon as unavoidably small due to remoteness? Surely just “rural” would do! Anyway a number of small rural hospitals are particularly challenged due to the difficulty of recruiting A&E staff. Whether the changes previewed here will make a difference remains to be seen. This article tells us:
Under a pilot scheme at small number of hospitals, the length of time every patient spends in A&E will be recorded, yielding an average waiting time, as has been introduced for ambulance waiting times.
It also includes the aim of treating every person who arrives at A&E experiencing a mental health crisis within an hour.
Since ending the four-hour target was first mooted it has raised fears that it could lead to patients being left untreated for hours, and concern that the move might be motivated by political expediency rather than patient safety.
NHS England, however, says it will ensure faster life-saving treatment for those with the most critical conditions, such as heart attacks, sepsis, strokes and severe asthma attacks.
Prof Stephen Powis, the national medical director for the NHS in England and the leader of the review, said: “Now is the right time to look again at the old targets, which have such a big influence on how care is delivered, to make sure that they take account of the latest treatments and techniques, and support, not hinder, staff to deliver the kind of responsive, high-quality services that people want to see.”
Labour introduced the measure in 2004, stipulating that hospitals had to treat 98% of A&E patients within four hours, before the coalition government reduced the target to 95% in 2010. It has not been met nationally since July 2015.
Full details:
https://www.theguardian.com/society/2019/mar/11/pilot-scheme-moves-nhs-closer-to-ending-four-hour-ae-target
400 care home operators collapse in five years as cuts bite
This article reveals a pressing need for a new approach to tackling the challenge of the current default position approach to the provision of adult social care. We know that some of the highest costs and most challenging areas for adequate provision are in rural settings. It tells us:
More than 100 care home operators collapsed in 2018, taking the total over five years to more than 400 and sparking warnings that patients in homes that close down could be left with nowhere to go but hospitals.
UK care home firms are buckling under the pressure of funding cuts, crippling debt and rising costs, according to research by the accountancy firm BDO.
It found that in the period between 2014 and 2016 there were an average of 69 care home company insolvencies per year. The number rose sharply to 123 in 2017 and another 101 collapsed last year.
Martin Green, the chief executive of the social care trade body Care England, called for urgent action to avoid a shortage of beds in a sector that provides care and accommodation for more than 410,000 residents.
“The situation is serious and getting more serious,” Green said. “The cost of care is ever rising and yet the amount of money local authorities pay for care is at very best rising much more slowly or not at all.
Full details:
https://www.theguardian.com/society/2019/mar/11/over-400-care-home-operators-collapse-in-five-years-as-cuts-take-toll
Junk food giants must stop marketing to children - or see their ads banned entirely, says health chief
It would be really useful to use data from public health England to show how the distribution of the obesity challenge breaks down between urban and rural places. This article tells us:
The World Health Organisation (WHO) said food giants are exploiting loopholes in regulations to bombard children with adverts on YouTube and Facebook.
And one of Public Health England’s advisers called for the rules to be redrawn - with advertisements for fatty and sugary foods banned entirely if children were found to be being exposed to them.
The call came as research from the University of Liverpool found three-quarters of under 16s are being exposed to such adverts on social media - despite rules which are supposed to protect them.
A new report by the WHO today warns that watchdogs are failing to keep pace with sophisticated marketing techniques used to promote junk foods to ever younger markets. It warns of “unequivocal evidence” that exposure to such products is fuelling a global obesity crisis.
In the UK, advertising authorities say that products high in fat and sugar can only be advertised if at least three quarters of the audience is adult.
But Nick Sheron, a clinical adviser to PHE, said these rules did not go far enough - calling for a ban on such adverts if children were found to be being exposed to them.
Full details:
https://www.telegraph.co.uk/news/2019/03/14/junk-food-giants-must-stop-marketing-children-see-ads-banned/
Private ambulances increasingly used by NHS ‘putting patients at risk’, damning report finds
This very worrying report raises the fundamental question of why we don’t have enough state provision to meet demand. I know you could say that’s true of every public service but this seems to me to be quite an acute example. The story tells us:
A damning report has warned that the increasing use of private ambulances is leading to examples of poor care, including a dialysis patient left to wander the streets.
Private ambulances are being used by the NHS more and more to transport patients to appointments and hospital, and to respond to emergency 999 calls.
But the Care Quality Commission (CQC) said it was concerned about the quality of care, staff training and use of medicines.
Inspectors gave a number of examples of poor practice, including one provider who was “based in a hotel room and did not store controlled drugs appropriately, a paramedic who had their drug bag under their bed in a B&B, and morphine books with pages missing, illegible entries and incorrect information”.
In another example of poor care, one provider was transporting dialysis patients with no policies in place, no monitoring of transport time, and no monitoring of fluid, nutrition or toilet breaks.
Check NHS cancer, A&E, ops and mental health targets in your area
This is a really useful tool for finding out how services are running from an NHS perspective in your area. The article tells us:
The NHS is under severe pressure. Rising numbers of patients need hospital care - whether in an accident and emergency department, for cancer treatment or for planned operations and care, such as knee and hip replacements. Growing numbers of people are also reporting they are struggling with their mental health.
For each there are strict targets local services are expected to meet across the UK. But what are the chances of being seen in time where you live? Use our interactive tracker [accessed through the web link above] to find out.
Full details:
https://www.bbc.co.uk/news/health-41483322
Other Stuff
Workforce
Dido Harding Chair of NHS Improvement is leading a workforce review and she is proposing that much more influence should be exercised locally an article in the HSJ tells us:
Local areas will be given much greater control over NHS workforce policy with responsibilities being devolved to local areas from national bodies, a letter to NHS chief executives has revealed.
Workforce implementation plan chair Dido Harding and national executive lead Julian Hartley said in a letter sent to chief executives yesterday that they would look to devolve more responsibility for workforce issues to sustainability and transformation partnerships and integrated care systems.
There will also be a review of how national bodies regulate trusts, with the letter making clear positive leadership in the NHS was not “consistently demonstrated across the system in national bodies, providers or commissioners” and there was a need to acknowledge this and “improve our leadership culture and capacity”.
Funding
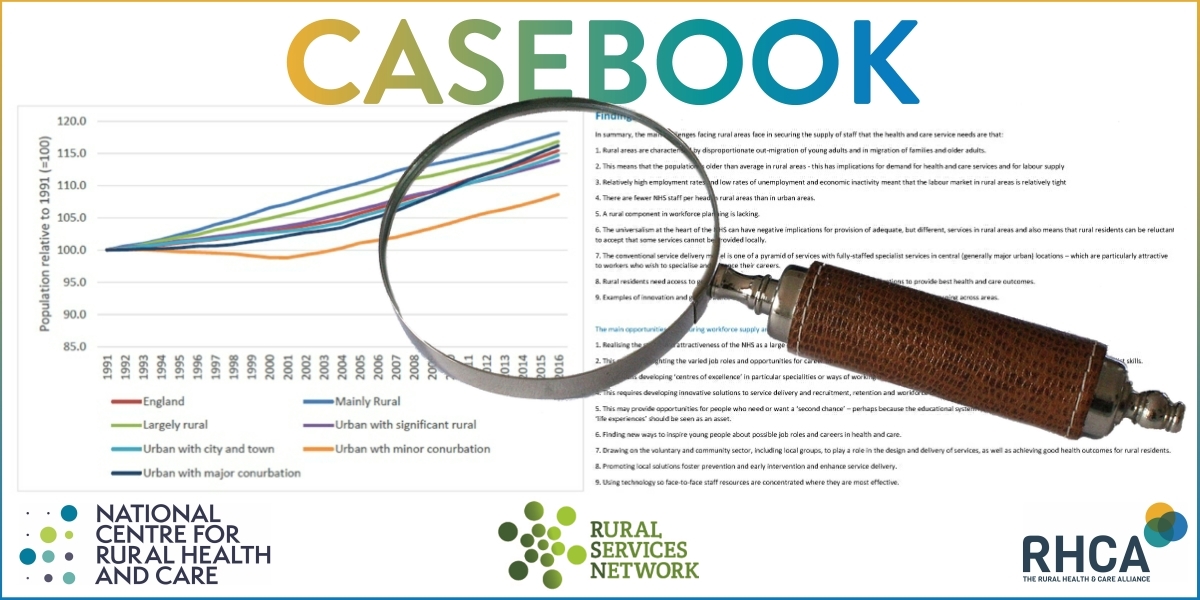
The National Centre for Rural Health and Care working with the Nuffield Trust has commissioned research, which shows that the most rural areas currently get a raw deal. This work was featured recently in the Sunday Telegraph and told us:
The research found that the funding situation has become so precarious that six of England’s smallest and most remote hospital trusts now account for nearly a quarter of the £1bn NHS provider deficit.
On average, at small remote hospitals just 84 per cent of patients were treated in Accident and Emergency within four hours, compared with 90 per cent of those in other trusts, the analysis found.
Just 79 per cent of those needing treatment began it within 18 weeks, compared with 85 per cent of those elsewhere.
The number of days lost to bedblocking was far higher in remote small hospitals, the analysis found, with 118 per 1,000 admissions, compared with 81 per 1,000 admissions in other trusts. And their average deficit was four times that of other trusts, the study found.
Researchers said NHS trusts in rural areas were facing cost pressures, which were not properly compensated.
This included difficulties recruiting staff, meaning higher reliance on costly agency staff, the study commissioned by the National Centre for Rural Health and Care found.




