T: 01822 851370 E: [email protected]
Visit RSN Survey about life in rural England to find out more.
Casebook - June 2019
In Casebook this month: the shocking impact of austerity, domestic abuse and its wider connection with mental health, Brexit and the NHS market, a Cornish GP charm offensive and the worrying ripples from county lines – plus some interesting other stuff including the emerging findings from Baroness Harding’s workforce review.
June 2019 Edition
In Casebook this month, rural obesity, children and mental health, the loss of a huge cadre of mental health nurses, growing levels of opiod addiction and spiraling rural local authority adult social care costs. Read on for more information
News
Austerity to blame for 130,000 ‘preventable’ UK deaths – report
This is hard hitting stuff which has a footprint in a number of rural communities.
More than 130,000 deaths in the UK since 2012 could have been prevented if improvements in public health policy had not stalled as a direct result of austerity cuts, according to a hard-hitting analysis to be published this week.
The study by the Institute for Public Policy Research (IPPR) thinktank finds that, after two decades in which preventable diseases were reduced as a result of spending on better education and prevention, there has been a seven-year “perfect storm” in which state provision has been pared back because of budget cuts, while harmful behaviours among people of all ages have increased.
Had progress been maintained at pre-2013 rates, around 131,000 lives could have been saved, the IPPR concludes. Despite promises made during the NHS’s 70th birthday celebrations last year to prioritise prevention, the UK is now only halfway up a table of OECD countries on its record for tackling preventable diseases
Full details:
Domestic abuse survivors 'more at risk of serious mental illness'
My gut would have told me that this is the case but its interesting to see it confirmed. A salutary tale here – this article tells us:
Women who experience domestic abuse are three times more likely to develop a serious mental illness, Birmingham University research suggests.
They are also twice as likely to have had some form of mental illness already, the study in the British Journal of Psychiatry found.
Experts said opportunities were being missed to detect abuse and support vulnerable women.
GPs said they were highly trained to spot it, but it was often well-hidden.
The study was based on 18,547 women who had told their GP of domestic abuse they had experienced.
They were followed up over a number of years and compared with a group of more than 74,000 women of a similar age who had no experience of domestic abuse.
Dr Joht Singh Chandan, lead author and academic clinical fellow in public health at the University of Birmingham, said the burden of mental illness caused by domestic abuse in the UK could be much higher than previously thought.
Full details:
https://www.bbc.com/news/health-48541604
Trump visit: Could US companies run NHS services after Brexit?
Radio 4 – the font of all knowledge – was trailing a story that there is an agenda post Brexit by pharma companies to get us to pay more for our drugs, driven in part by US interests. Anyone who thought the NHS was immune from the commercial (as opposed to the workforce issues which have been heavily discussed already) should read this
Along with the pomp, protests and politics, President Trump's visit to the UK brought renewed debate about whether a post-Brexit trade deal between the two countries could involve opening up the NHS to US companies.
Mr Trump told a press conference: "When you're dealing with trade, everything's on the table - so the NHS or anything else".
He quickly rowed back, saying he did not consider the NHS to be part of trade - though not before MPs from across the political spectrum had come out to say the health service was "not for sale".
The question is what "for sale" would actually mean.
As health think tank the Nuffield Trust points out, "a trade deal would not have the power to stop the NHS being a free, universal service".
But could greater market access to the health service for US companies be up for negotiation?
The NHS is funded by government through taxes. Decisions about how to spend money and how to deliver care are made by public bodies, not operating for profit.
But there are already various opportunities for private companies - including US firms - to win business within the NHS.
Out of a budget of more than £120 billion a year, 7.3% was spent on private providers in England in 2017-18, according to government accounts. That's up from 5.3% in 2011-12.
All drugs and equipment have to be bought from the private sector, and the UK imports about £2bn of pharmaceutical products a year from the US - 9% of total drug imports in 2018.
Full details:
https://www.bbc.com/news/health-48527328
Cornish village hopes to charm new GP into taking over practice
Now this is an excellent example of rural people power in action. At the 4th session of the Parliamentary Inquiry into Rural Health and Care on Thursday Professor Stephen Singleton was talking about a very similar approach in a Cumbrian example. The key point here is that health and care needs significant community engagement if it is to be sustainable in the long term in many small rural towns. This story tells us:
Lorna Cavanagh can name every doctor who has worked at the surgery in the Cornish fishing village of Mevagissey since 1944 – the year she was born. The 75-year-old describes calling a Dr Hannon at 2am when her sister-in-law was taken ill with kidney stones in the 1970s. “You could see him from our window coming down that hill on his moped,” she said. “It was a very personal service.”
Last month the well-respected partner of the local practice, Dr Katherine James, announced she would be handing back her contract to run the surgery on 31 July. NHS England says it is assessing the options available, but it is feared the much-loved community surgery could close and its 5,300 patients forced to use the infrequent and expensive bus service to travel elsewhere for treatment.
Faced with this prospect, the residents of Mevagissey, which is eight miles south of St Austell, the nearest medium-sized town, took matters into their own hands. The “Will you be my GP?” campaign – with its #willyoubemygp hashtag – aims to persuade doctors around the country that they should make the picturesque fishing village, with its narrow winding streets and superior fish and chips, their home. In a campaign video posted on the Cornwall Channel, a crowd of residents chant: “Be our GP. We are a lovely community. We need you.”
Full details:
Police say they lack resources to tackle county lines drugs networks
This is a huge public health issues (like knife crime – to which it is related) and makes you think about where we draw the line (pun intended) in social policy between health and civil (in this case crime) issues. The story tells us:
Police have now identified around 2,000 drug supply chains as part of the county lines network, which is fuelling knife crime as rival gangs clash, while a majority of police forces say it is also linked to an increase in gun crime.
A £3.6m National County Lines Coordination Centre, jointly run by the National Crime Agency and the National Police Chiefs’ Council, opened last September. It aims to improve intelligence on county lines across forces and improve safeguarding, while better protecting victims. During a single week in late May, police targeting county lines gangs arrested about 600 people suspected of involvement in drug dealing following operations coordinated by the centre. But with almost one in 10 people in the UK taking drugs in the last year, and the number of 14- to 18-year-olds convicted for possession with intent to supply in England and Wales rising by more than two-thirds in five years, there are growing calls for a different approach.
Leaving a county lines gang is often dangerous, but by “being there and really sticking by that young person’s side”, St Giles says it gives people a fighting chance to avoid being lured – or forced – back into a life of crime. In Coventry and Wolverhampton, the charity’s caseworkers – often former gang members – will sit at the bedside of young people, predominantly boys, who have been stabbed to offer them support and guidance. Many have been involved in gang feuds, sometimes drug-related, and are extremely vulnerable.
Full details:
Other Stuff
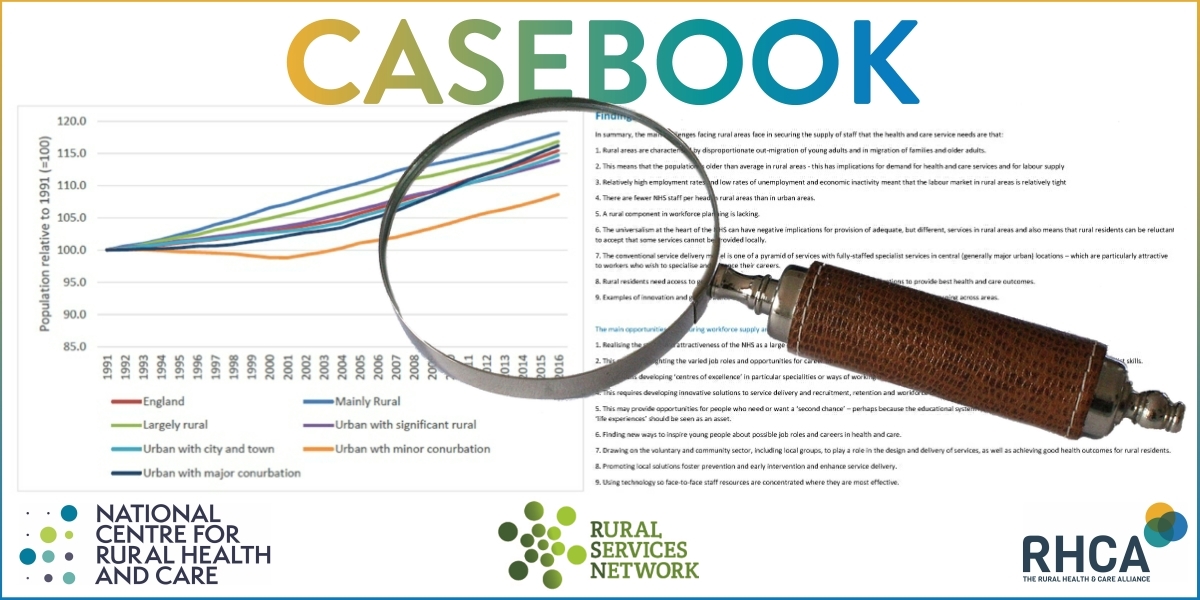
- Baroness Harding’s new work on workforce issues has been released, without much public attention. It also says too little about rural issues from my point of view. You can read it here:
https://www.longtermplan.nhs.uk/wp-content/uploads/2019/05/Interim-NHS-People-Plan_June2019.pdf - We had an excellent time at the 4th session of the Parliamentary Inquiry into Rural Health and Care on Thursday last. We had evidence from the Chief Nurse, BMA, Royal College of Nursing, Somerset and Devon Councils, West Suffolk NHS Foundation Trust and the Cumbria Learning and Improvement Collaborative. All talking about training and recruitment. Details will soon be published here:
https://www.ncrhc.org/




